The Importance of CGMs in the Management of Diabetes
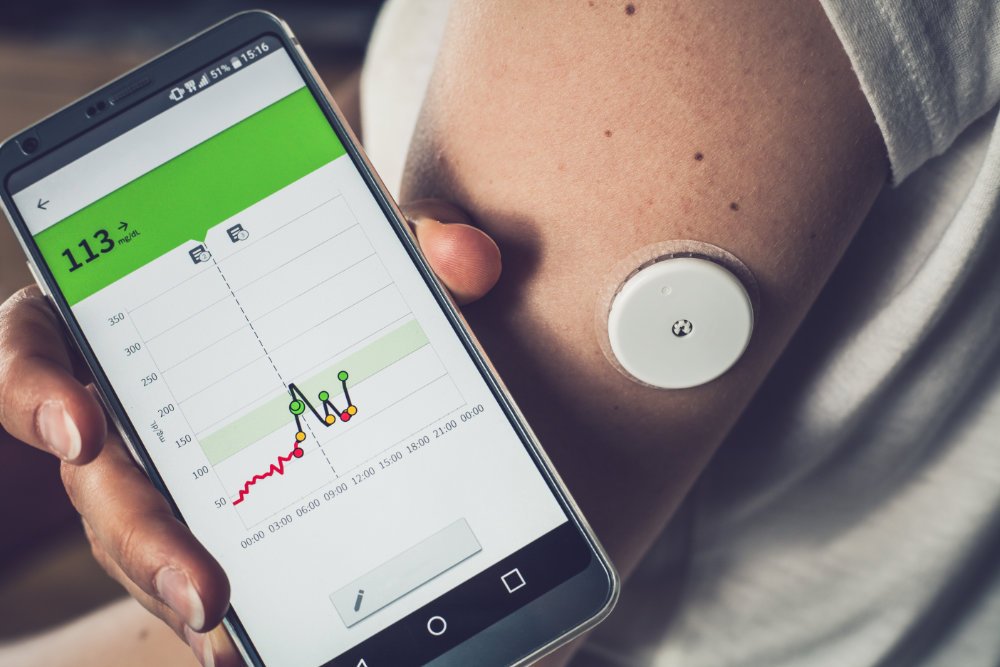
A continuous glucose monitor (CGM) is a wearable device that tracks blood glucose every few minutes while worn. They include a small disposable sensor worn under the skin (often on the arm or stomach) which transmits data to an attached transmitter and receiving device. These devices allow individuals with diabetes to constantly monitor their blood sugar levels, providing real-time data and insights into how their body is responding to different meals, activities, and medications. This data can be viewed by the patient, their family, or the care team – depending on the permissions outlined in the application and make for an excellent source of data for Remote Patient Monitoring (RPM) programs.
Benefits of CGM Devices and Improved Blood Glucose Monitoring
Continuous blood glucose monitoring allows individuals living with diabetes to get a complete picture of their blood sugar control. The improved visibility allows patients and their care teams to make better short and long-term treatment decisions resulting in improved health outcomes.
One of the biggest benefits of CGM devices is the ability to track glucose levels throughout the day and night, which can help individuals with diabetes identify patterns and trends that they may not have been aware of before. For example, a CGM device may reveal that a person's blood sugar levels drop rapidly at night, indicating that they may need to adjust their insulin doses or bedtime snacks.
Another benefit of CGM devices is the ability to alert individuals with diabetes to potential problems, such as high or low blood sugar levels. This can help prevent dangerous short-term complications such as hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). In addition, by addressing health issues early, it helps prevent longer-term complications such as vision loss or lower-limb amputation. For example, some CGM devices can be set to send an alert to an individual's phone or watch if their blood sugar levels drop below a certain threshold. These alerts can also be set up to be sent to the family of the patient and their care team. This improves overall visibility into the condition of the patient and promotes better health outcomes.
In addition to the above, patients using CGMs utilize less needles to test their blood glucose levels. Patients only need to manually test their blood twice a day to calibrate the device, once in the morning and once before bed. This drastically reduces the amount time blood is drawn from the fingers and results in reduced pain and soreness in the hands.
How CGM Devices Are Changing Diabetes Management
CGM devices are also beneficial for healthcare providers, as they can provide real-time data on an individual's glucose levels, which can help inform treatment decisions. One of the problems with manually testing blood glucose is that your doctor has no way of viewing your trends unless you write them down and present them in your next visit.
For example, a healthcare provider may use data from a CGM device to adjust an individual's insulin regimen or to identify potential problems with their diabetes management. Having an enhanced level of data at the clinician’s fingertips is vital to improving care as it allows for more frequent and preventative treatment adjustments. By empowering both the patient and the provider with improved data, better outcomes for the patient are promoted.
CGMs and Remote Patient Monitoring
Another advantage of CGM devices is when they are integrated into a remote patient monitoring program. The power of having a CGM device, smart scale, blood pressure monitor among other devices packaged together with data synced to a clinician dashboard cannot be understated. These devices, when working together, can provide a holistic view of the patient and can go even further in improving treatment and management than with a CGM alone.
We are proud to offer industry leading CGM devices through Dexcom and FreeStyle Libre on the Mozzaz Platform. In addition to the benefits remote patient monitoring can bring, we offer some additional tools such as our nutrition analyzer – where patients can easily input their daily meals and have corresponding calories and macronutrients stored. As well as our health 360 which can draw environmental conditions and overlay them with patient’s biometric readings.
In Conclusion
Overall, CGM devices are changing the way that diabetes is treated and managed. They are providing individuals with diabetes valuable insights into their glucose levels and enabling healthcare providers to make more informed treatment decisions. When they are combined into RPM programs, they enable a true holistic patient view which helps to improve patient outcomes.
It's worth noting that CGM devices are not meant to replace traditional blood glucose monitoring methods but are rather a supplement to them. As mentioned in the article, it's important for people with diabetes to continue to check their blood glucose levels with a traditional glucose meter as well.
As technology continues to evolve, it is likely that CGM devices will become even more advanced, providing even more benefits for those living with diabetes and their care teams.
If you are interested in utilizing CGM devices in your current or upcoming RPM program, contact us today for a consultation.